Intro: Imagine your brain’s communication system as a complex highway where chemical messengers dictate hunger, fullness, and emotional balance. Eating disorders create dangerous detours on this vital pathway.
Part 1: The Chemical Conversation in Healthy Brains
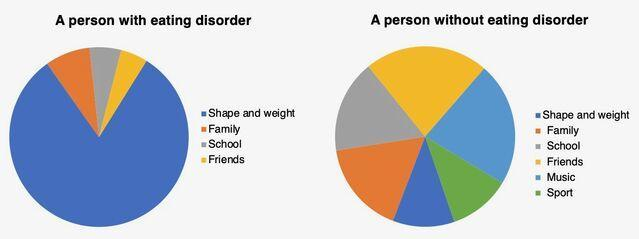
Our brains constantly send messages about hunger and satisfaction through neurotransmitters—tiny chemical couriers traveling between nerve cells. When your stomach empties, ghrelin (often called the “hunger hormone”) whispers to your brain’s hypothalamus: “It’s time to eat.” As you enjoy a meal, dopamine releases gentle waves of pleasure, rewarding you for nourishing your body. Meanwhile, serotonin helps maintain emotional calm and signals fullness. This elegant dance ensures we eat when hungry and stop when satisfied. For most people, finishing a comforting meal brings that warm sense of contentment—a sign these messengers are working in harmony. The system naturally balances cravings for different nutrients too; ever notice how after days of heavy meals, your body suddenly longs for crisp vegetables? That’s your neurotransmitters wisely guiding your nutritional needs.
Part 2: When Anorexia Mutes the Signals
In anorexia nervosa, the brain’s hunger alarms become dangerously ignored. Imagine ghrelin desperately shouting “We need fuel!” while the disorder installs soundproof walls. Studies show chronically starved brains actually produce more ghrelin, yet sufferers describe feeling no physical hunger—a terrifying disconnect. Dopamine pathways get rewired: Where food once brought pleasure, anxiety now floods the system at mealtimes. Sarah, recovering after three years of anorexia, recalls: “Seeing a plate of pasta felt like confronting a snarling beast, not dinner. My mind translated every hunger pang as proof of ‘control.'” Simultaneously, serotonin function declines, amplifying depression and obsessive thoughts about food avoidance. This neurotransmitter disruption creates a self-perpetuating cycle: Starvation damages the brain regions responsible for recognizing hunger, making recovery feel like learning to read vanished road signs.
Part 3: How Binge Eating Disorder Overrides the Brakes
Binge eating disorder (BED) represents a different system malfunction—like jammed accelerator pedals on satisfaction signals. Where healthy brains release dopamine gradually during eating, BED creates brief, intense surges that demand constant stimulation. “It wasn’t about taste,” explains Michael, who managed BED for a decade. “I’d eat until my stomach ached, chasing a fleeting calm that vanished immediately after.” Serotonin imbalances worsen this; low levels reduce impulse control while increasing cravings for carbohydrates (which temporarily boost serotonin). Crucially, the hypothalamus’ fullness signals get drowned out. Leptin—the hormone announcing “We’re full!”—becomes less effective, creating a physiological need for larger food volumes to trigger satisfaction. Many describe a dissociative state during binges: “It’s like watching someone else eat while your brain screams ‘Stop!’ but your hands keep moving.” This isn’t weak willpower; it’s a hijacked neurochemical reality.
Part 4: The Healing Pathway Forward
Recovery involves gently retraining the brain’s communication network—a process demanding patience and professional support. Nutritional rehabilitation comes first: Consistent, adequate nourishment repairs the physical infrastructure of neurons starved of essential fats and glucose. Cognitive Behavioral Therapy (CBT) helps rebuild healthier thought patterns, literally creating new neural connections. Mindfulness practices teach awareness of true hunger/fullness cues that were long ignored or feared. James, two years into recovery from bulimia, shares: “Learning to pause and ask ‘Am I physically hungry or emotionally empty?’ felt impossible at first. Now it’s my compass.” Crucially, restoring balanced neurotransmitter function reduces the overwhelming anxiety and depression that maintained the disorder. While medication like SSRIs may help correct serotonin imbalances temporarily, lasting healing comes from holistic self-care practices: Regular sleep stabilizes ghrelin; omega-3s support neuron repair; joyful movement rebuilds dopamine responses unrelated to food restriction. This isn’t erasing the disorder’s neural pathways but building alternative routes strong enough to bypass them.
Conclusion
Eating disorders create profound changes in the brain’s chemical language, making hunger unrecognizable and satisfaction unreachable. Yet neuroplasticity—the brain’s remarkable ability to rewire itself—offers powerful hope. Recovery is the courageous work of clearing the communication lines between body and mind, restoring trust in your own hunger signals. Every nourishing meal, every moment of self-compassion, gently reclaims your brain’s biological wisdom.